- Acknowledgements
- Introduction
- I. Achieving Family/Professional Partnerships
- II. Early and Continuous Developmental and Medical Screening for Autism
- III. Access to All Needed Autism Spectrum Disorder (ASD) Health, Mental Health, Education, and Social Services.
- IV. Organization of Community-based Services for Easy Use
- V. Youth transition to adult services, work, and independence
- VI. Appropriate Financing of Care
Acknowledgements
The ASD Services Roadmap was developed by the ASD Expert Working Group (EWG), a panel of autism experts established by the Services Subcommittee of the Interagency Autism Coordinating Committee in July 2004. The EWG is a diverse group comprising of members with special ASD expertise—service providers, educators, community program coordinators, researchers, individuals with ASD, and family members of individuals with ASD. The EWG was asked to review the state of the field and identify principles of best practices, challenges, and recommendations to provide the blueprint for a national public and private implementation plan for expanding and improving ASD services. The Services Subcommittee, Co-Chaired by Merle McPherson, M.D. and Sybil Goldman, M.S.W., provided general guidance to the EWG, however, the content and recommendations in this report were independently developed by the EWG. The preparation of this report was conducted under contract with Social & Scientific Systems of Silver Spring, Maryland.
- Sue Baker
Autism Services Consultant
- Margaret Bauman, M.D.
Community Health Provider
- Maggie Bishop
FICC Family Representative
- Nancy DiMauro
North American Family Institute
- Gay Finlayson
New Mexico Adolescent Program
- Sherry Glied, Ph.D.
Columbia University, School of Public Health
- David Holmes, Ed.D.
President, Eden Services and Institute
- Chris P. Johnson, M.D.
The Village of Hope, Children with Disabilities
- David Mandell, Ph.D.
University of Pennsylvania
- Gary Mesibov, Ph.D.
Director, Division TEAACH
- Scott Myers, M.D., F.A.A.P.
Giesinger Medical Center
- Cathy Pratt, Ph.D.
Indiana Institute on Disability and Community
- Ilene Schwartz, Ph.D.
University of Washington
- Stephen Shore
ASD Expert
- Stuart Spielman, Esq.
Community Services for Autistic Adults and Children
- Fan Tait, M.D.
Utah CSHCN State Program Director
- Amy Weatherby, Ph.D.
Florida State University Speech Pathologist
- Expert Working Group Consultant:
Beth D. Roy, M.S.
Social & Scientific Systems
Introduction
The increased number of children and adults diagnosed with ASD is a growing and urgent concern for families, service providers, and policy-makers, as the nation's existing health, education, and social service systems struggle to respond to the service needs of this population in a comprehensive manner. Though a number of effective services and funding options for individuals with ASD exist, they tend to be scattered, fragmented, and poorly coordinated. There are no widely accepted or implemented service guidelines for ASD, and there are significant gaps in knowledge about ASD among the professionals serving these individuals. Even where services are available, public and private financing are often inadequate to meet the needs of most individuals with ASD and their families. The success and well being of individuals with ASD and their families are affected by, and in large part, depend on communities and their resources. Thus, we must respond by developing community systems that are integrated across service sectors and are collectively responsible for achieving appropriate individual, family, and community outcomes.
In an effort to address these issues, the Interagency Autism Coordinating Committee (IACC) established a Services Subcommittee to develop a national action plan for ASD service development and delivery. The Services Subcommittee is comprised of officials from The Department of Health & Human Services and Department of Education agencies on the IACC, as well as parent/guardian members, with a mission related to assuring health, mental health, education, social and family support services. A designated lead from each agency sits on the subcommittee, however, they are supported by a host of other agenda staff and colleagues. The subcommittee's charge was to develop an action plan to address the immediate service system needs of individuals with autism and their families across the lifespan, based on the best available science and the best practices currently in use. As critical findings from ongoing and future clinical and health systems research strengthen the evidence base, these results can then be translated into services that meet the specific needs of individuals with ASD and their families.
The action plan, or "ASD Services Roadmap," is intended to provide a national blueprint to enhance existing systems; expand services for children, youth, and adults with ASD and their families; and coordinate services across systems. The Roadmap was developed in the context the President's New Freedom Initiative (NFI), and based on Executive Order No. 13217, "Community-Based Alternatives for Individuals with Disabilities," which calls upon the federal government to assist states and local jurisdictions to implement swiftly the decision of the United States Supreme Court in Olmstead v. L.C., which states that "The United States is committed to community-based alternatives for individuals with disabilities and recognizes that such services advance the best interests of the United States." Thus national impetus exists, through NFI, to reduce barriers to community services and independent living for all individuals with disabilities, including those with ASD.
As part of the NFI, HRSA's Maternal and Child Health Bureau was identified as the lead agency for "developing and implementing a plan to achieve appropriate community-based services systems for children and youth with special health care needs and their families." The Roadmap is built around the six performance measures for community systems of service outlined by the President's New Freedom Initiative (NFI):
- family and professional partnerships;
- early and continuous developmental and medical screenings;
- availability of all needed health, education, and social services;
- organization of community-based services for easy use;
- effective youth transition to adult services, work, and independence;
- access to adequate public/private insurance or other financing mechanisms.
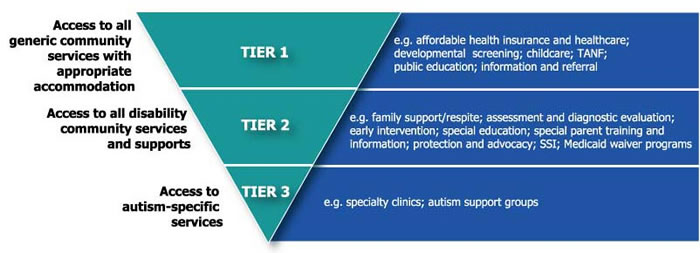
The Roadmap is further based on the premise that all individuals, including those with ASD deserve to grow, learn, live, and work in inclusive communities where differences are respected and needs met. The Roadmap embraces the model (Figure 1), which assures that individuals with ASD have access to the broad range of community services, including those available to all individuals, to individuals with disabilities and chronic conditions, and to services that are uniquely required to address ASD.
Figure 1
Ultimately, the intent of the Roadmap is to incorporate ASD service initiatives for children, youth, and adults with ASD into the existing Federal mechanisms for community-based systems of services for all individuals with special needs. The Roadmap incorporates the wide range of public, private, and voluntary partnerships needed to improve ASD services.
In order to effectively and efficiently address this need, in the summer of 2004 the Services Subcommittee (SS) of the IACC established a panel of experts from different fields to provide recommendations. This diverse group, called the Expert Working Group (EWG), consists of members with special ASD expertise--service providers, physicians, educators, community program coordinators, researchers, individuals with ASD, and family members of individuals with ASD. The EWG was asked to review the state of the field and provide recommendations for expanding and improving ASD services.
The EWG was provided with a list of discussion topics and asked to provide 1) their recommendations on the principles of best practice, 2) significant constraints to reaching these levels of best practice, and 3) strategies for action and implementation of these best practices nationwide in each area. After submitting their responses, the EWG reviewed the input from all of the members in all of the areas, and met to discuss and refine the compiled information. The EWG identified a number of urgent cross-cutting themes and major recommendations:
- Address urgent need for services across the lifespan;
- Coordinate services across the multiple systems serving individuals with ASD so that families can easily access services;
- Increase provider capacity from primary care through specialty care;
- Develop standards of care for screening, diagnosis, treatment and other services
- Expand public and private financing mechanisms to ensure that individuals and their families can access ASD services;
- Work at the state and community level to foster creative approaches to expand service capacity to match local needs.
Input of the EWG, guided by IACC members affiliated with Health Resources and Service Administration (HRSA), Substance Abuse and Mental Health Services Administration (SAMHSA), National Institute of Mental Health (NIMH), and the Autism Society of America (ASA), was the basis for a draft ASD Roadmap. Representatives of the EWG presented a status report to the IACC at the November 19th, 2004 IACC meeting, at which time the IACC approved of the progress to date, and endorsed the plan to continue efforts of the Services Subcommittee and Expert Working Group to develop a final ASD Roadmap and Implementation Plan for presentation at the May 2005 IACC meeting. It is expected that the ASD Services report will serve as a companion to the IACC Research Matrix, submitted in an April 2004 report to Congress.
This summary provides a synthesis of the issues, challenges, and recommendations for actions to address each of the six performance measures for community systems of service.
I. Achieving Family/Professional Partnerships
Achieving effective and active partnerships between individuals and families with autism spectrum disorder (ASD) and professionals who provide ASD services is fundamental to achieving family-centered, coordinated quality care. It is vital that professionals value and respect the pivotal role of individuals and families with ASD in systems of care and listen closely to the experience of families who deal with ASD on a daily basis. Individuals and families with ASD are the ultimate decision-maker for their care and their input is critical to a mutually agreed upon plan of care. Professionals require training and expertise in ASD to provide quality evaluation, skilled treatment, and knowledgeable referrals to other ASD community resources. A trusting relationship between families and professionals is built on mutual respect and clear and effective communication of information about family support needs and the availability and gaps in ASD resources. Individuals, families, and professionals should receive support and training in order to achieve the goal of effective family/professional partnerships.
ASD can overwhelm families and professionals and test the endurance of all who are involved in care and support. The day-to-day realities can drain family resources and limit the time available to devote to becoming skilled family advocates and to building collaborative professional partnerships. This is especially true for families with limited economic resources and cultural barriers, but all families require support in developing the skills and knowledge to inform and affect provider systems. The intensity and complexity of ASD service needs can be a disincentive for some professionals to engage in ASD care, especially when financial compensation is not adequate for the time involved. These stresses and pressures on families and professionals create barriers that must be overcome in order to achieve the goal of full family participation in decision-making and mutual family/professional partnerships.
Progress has been made in developing family-centered supports and services that are designed in such a way that parents and professionals are partners in developing these services and supports needed for children with special needs. ASD presents unique challenges in this regard because of limited knowledge of the disorder and the broad impact that ASD has across the life cycle. In building the capacity for family/professional partnerships, it is important to support bridges and transitions across the life cycle.
Goal: All individuals with ASD and their families will have a well-established, trusting, and mutually respectful relationship with a healthcare professional (medical home) who listens and responds to concerns, and who acts as an equal partner in providing a clearly defined plan of coordinated services.
Challenges:
- Lack of time, knowledge, support, and training.
- Lack of understanding and communication regarding ASD.
- Individuals with ASD and their families may not have a well-established relationship with a primary healthcare professional and a medical home to respond to concerns and coordinate care.
Recommendations:
- Provide ongoing training and technical assistance for professionals and families to engage as full partners.
- Increase ASD information and education resource capacity at national and local levels.
- Integrate ASD into existing initiatives to strengthen family support and involvement and to establish integrated systems of care.
II. Early and Continuous Developmental and Medical Screening for Autism
Early screening followed by timely comprehensive ASD assessments and appropriate referral to coordinated developmental, educational, medical and family support services is critical. Screening and diagnosis should occur as early in life as possible. The symptoms of ASD appear before age three, by definition, and ASD can sometimes be diagnosed as early as 18 months; however, children are often not diagnosed until they are of school age. Early diagnosis and treatment lead to better long-term outcomes, as well as a positive impact on the overall quality of life for individuals with ASD and their families. ASD diagnosis can provide eligibility and reimbursement for early intervention and education, and numerous other health, mental health, and social service programs. Once a diagnosis of ASD is made, genetic counseling about the risks to siblings and subsequent children can potentially be provided. The goal of early and continuous developmental and medical screening followed by comprehensive services can be met by raising public awareness and knowledge of ASD, standardizing and improving the practice of ASD screening, and strengthening systems to make early identification, diagnosis and services routinely available.
Much progress has been made in the past 20 years in early diagnosis of ASD and detection of underlying etiologic neurologic and genetic conditions. There are, however, still major gaps in the public and provider knowledge, and widely accepted and practical screening methodologies are still in development. Early and continuous screening and diagnosis of ASD are especially challenging because autism is a complex disorder of brain development that spans a broad continuum, from mild social and communication deficits to severe developmental and behavior conditions. Due to a lack of knowledge and training, providers are often not comfortable with ASD screening methodologies and care and providers sometimes lack time and reimbursement needed to fully address the individual and family concerns. Providers are concerned that if a diagnosis is made, there is not a system of services available to adequately meet the need. Universal and systematic early identification, followed by referral into coordinated service systems, is still a goal, not a reality.
Recent research confirms what may be obvious to many; parents are usually correct in their concerns about their child's development and are the first line of surveillance for ASD in children. Early diagnosis of ASD in children is highly dependent on professional's listening to the parents' concerns and implementing basic screening methods that can be administered and interpreted without extensive training. There are a variety of screening methods that have been developed, but they are still being refined to improve their sensitivity, standardize results, and develop practical and effective models of implementation. The best practice is for providers to fully engage the individual and family with ASD as a partner in identification and diagnosis, to have the training and tools to monitor developmental, social, behavioral, and medical issues, and to participate as part of the team in making ASD early identification and treatment a routine part of care.
Goal: Universal early identification of signs of ASD, followed by appropriate referrals to a coordinated and comprehensive service system.
Challenges:
- Lack of awareness, time, and training of medical and developmental providers leads to the lack of regular and standardized screening.
- Inadequate screening and diagnosis methods and capability.
- Inadequate linkage to the referral resources and service network.
- Inadequate reimbursement to adequately compensate providers for screening.
Recommendations:
- Support IACC Screening Subcommittee efforts to increase public awareness and incorporate ASD into routine screening.
- Develop guidelines for ASD screening, diagnoses, and referral for follow-up.
- Improve and standardize developmental and ASD screening methodologies.
- Incorporate ASD guidelines into curriculum for residency, professional certification, and other training programs.
- Promote linkages between medical homes and existing resource networks for developmental, educational, rehabilitative, social, and specialty services for ASD.
- Provide technical assistance and disseminate educational materials, checklists, implementation tools for ASD screening to families and professionals.
III. Access to All Needed Autism Spectrum Disorder (ASD) Health, Mental Health, Education, and Social Services.
Individuals with ASD require a comprehensive range of health, mental health, educational, and social services. The service requirements of individuals and families with ASD are intense and require a long-term and year-round approach to address chronic needs. ASD requires a holistic and multi-disciplinary approach to services and supports in order to provide a coordinated approach to address the broad range of needs of children, adolescents, and adults with ASD. There are significant individual differences and unique service needs that vary throughout the life cycle; however there is a critical need for a consistent definition of ASD services with guidelines that establish the framework for a quality standard of services to be provided in a consistent way and to ensure that services are adequately covered and paid for through private and pubic mechanisms.
There is a serious and persistent lack of adequate capacity to provide appropriate care for children, adolescents, youth, and adults with ASD. There are many factors that contribute to this serious deficit in provider capacity; however, lack of appropriate funding and reimbursement for ASD service providers is a major factor. Also, as an emerging and still not well-understood medical disorder, ASD has not received the academic and research focus to attract adequate numbers of health professionals who are adequately trained to specialize in the field.
Although serious gaps exist in provider capacity to meet service needs at all stages of the life cycle, gaps in the availability of services for adults with ASD are most glaring and urgently in need of attention. When individuals with ASD are no longer eligible for early intervention and school-based special education services, less than meager services are available. There are even fewer services available for higher functioning youth and adults.
Unlike health conditions for which there are specific treatment protocols based on research that have been incorporated into curriculum and provider reference materials, there are no widely accepted guidelines for ASD to assist providers in the management of ASD treatment. Providers at specialty medical centers are best informed about the latest research results and currently accepted strategies, but without guidelines of care, primary providers are faced with a challenging task of diagnosis and treatment. There are better-defined treatment models for early developmental interventions for young children screened and diagnosed with ASD. Any child younger than 3 years of age with a known developmental disability or demonstrated developmental delay is eligible for early intervention through Part C of the Individuals with Disabilities Education Act (IDEA) which includes developmental, therapeutic, communication, social interventions, and family training and support services. After age 3, children may be eligible for pre-school and school-age special education programs which provide children with social skills, functional communication, and learning skills.
Goal: Individuals and families with ASD have ready access to integrated and coordinated health, mental health, education, and social services provided by well-qualified ASD providers throughout the life cycle.
Challenges:
- Lack of adequately trained providers.
- Inadequate time, resources, and reimbursement.
- Lack of education, training, and support for families and multi-disciplinary professionals.
- Lack of services and coordination across existing services.
Recommendations:
- Promulgate and promote use of ASD practice guidelines to define standards of care in health, mental health, social services, and education.
- Incorporate ASD service guidelines into curriculum for residency, professional certification, and other pre- and in-service training.
- Provide incentives to ensure greater availability of well-trained providers and a more equitable distribution of services across geographical areas.
- Develop an action plan for collaboration at all levels to identify services and address the service needs of persons with ASD within the broader initiatives to develop community-based systems of services for all persons with disabilities.
IV. Organization of Community-based Services for Easy Use
All individuals, including those with ASD, deserve to grow, learn, live, and work in inclusive communities where differences are respected and needs met. Executive Order No. 13217, "Community-Based Alternatives for Individuals with Disabilities," calls upon the federal government to assist states and localities to swiftly implement the decision of the United States Supreme Court in Olmstead v. L.C., stating "The United States is committed to community-based alternatives for individuals with disabilities and recognizes that such services advance the best interests of the United States." The national impetus exists, through the President's New Freedom Initiative, to reduce barriers to community services and independent living. It is clear that the success and well-being of individuals with ASD and their families is affected by, and in large part, depends on communities and their resources. For maximum benefit, community services must be organized in ways that recognize the interconnected role of physical health, developmental processes, and emotional well-being in shaping individual and family outcomes, and respond by developing community systems that are integrated across existing service sectors and collectively responsible for achieving individual, family, and broader community outcomes.
The complex needs of individuals with ASD and their families require a range of services that inevitably cross agencies and funding sources. In addition to ongoing issues related to appropriate type and intensity of treatments and interventions for individuals with ASD and their families, a myriad of significant systems constraints exist in the way that services are currently organized and provided at the community level, and supported, or not, by policies at the State and Federal level. Most community service systems are characterized by multiple service programs, each with their own funding streams, eligibility requirements, policies, procedures, and service sites. Communities often lack sufficient services, and those that do exist are often distributed in an inequitable manner. The consequence is a system of service that is unresponsive, fragmented, and difficult for both individuals and families to navigate. Furthermore, service availability is not consistent across the U.S., varying from state to state and within state geographic areas. For example, services in rural areas are often especially deficient. Services and supports should be financially and geographically accessible to all who need them and there is a critical need for mechanisms to facilitate access and integrate care across systems, resulting in consistent and user friendly access to all services.
Traditional divisions that often exist between these systems and providers can be especially disruptive for individuals with ASD. Even when receiving multiple services from many sources, individuals and families may in fact, not be receiving the services they need the most. Fragmentation within the system results not only in less than adequate services for individuals and families, but also in the inability of the community to address the problem. Because information is scattered across a wide number of unconnected programs and sources, communities lack the knowledge, data, and capacity to understand and act upon the problem from a service integration perspective.
No one agency, department, or intervention alone can guarantee achievement of desired outcomes for the individuals and families it serves. An effective community-based system of services operates across service sectors. It facilitates the integration of services in several dimensions, including organization, delivery, and financing. A community-based system of services refers to the framework within which a variety of programs work together to meet the many, varied needs of the individuals it serves. Development of community-based systems of services requires that their governance, planning, and management involve key community stakeholders. It is equally critical that linkages be forged between federal and state agencies, and between public sector and private sector to promote, support, and advocate for systems development at the community level. To organize community services in a family centered way, stakeholders must engage in capacity building, including the enhancement of leadership and collaboration skills among key community stakeholders. Federal and state governments and national and regional foundations can play valuable roles in this effort by fundamentally redefining and restructuring technical assistance and education to make them more responsive to the needs of local communities.
Goal: Community-based services will be organized so that individuals with ASD and their families can use them easily.
Challenges:
- Ineffective integration of ASD services into broader system of care.
- Lack of interagency coordination.
- Lack of access to information.
- Lack of time, resources, and reimbursement.
Recommendations:
- Support family-driven state and community development initiatives to implement creative approaches to effective practice.
- Provide technical assistance to states and communities to implement effective service delivery models.
- Provide a user friendly web based resource for ASD families and providers that includes information on ASD, successful screening and community service models, ASD providers, research, etc.
- Ensure that individualized plans coordinate a comprehensive continuum of services and supports across the lifespan, and across all necessary service sectors.
- Identify and analyze effective models that organize, integrate, and deliver comprehensive services.
- Develop models that permit providers and families to have systematic access to shared provider records and examples of exemplary practice.
V. Youth transition to adult services, work, and independence
ASD is a disorder that extends across the lifespan from early childhood throughout adulthood. Few coordinated services have been made available to assist youth and young adults diagnosed with ASD transition from school to work, home to independent living and from child and family-centered care to adult-centered care. The goal of transition is to provide health, education and social services that are uninterrupted, coordinated, developmentally appropriate and psychologically sound prior to and throughout the transfer into the adult system of services. Transition planning services should begin early with initial diagnosis. Successful transition to adulthood is determined by continuity and use of appropriate health care and community-based services, as well as by the maintenance of heath and well-being of the young person with ASD.
Youth with ASD and their families often face significant and seemingly insurmountable challenges to making successful transitions into adulthood including a lack of well trained and prepared adult service providers, inadequate funding mechanisms for the coordination of adult services, poor skill development for employment and independence, and an overarching lack of awareness of the changing service needs of persons with ASD across the lifespan. As a result of this lack of focused, coordinated, well-funded services, many youth and young adults with ASD are forced to remain dependent on family members, pediatric service providers, and public programs such as Supplemental Security Income (SSI), Welfare, and Medicaid rather than having access to opportunities that will enable them to become independent and remain healthy well into adulthood.
Collaboration between the service system and youth and young adults with ASD leading to dedicated funding of transition services in health, education, and employment beyond the age of 21 is essential to the delivery of a comprehensive, coordinated set of services that are age appropriate and delivered across the lifespan and in a manner in which youth and their families can easily access them.
Goal: All individuals with ASD will receive the services necessary to make transitions to all aspects of adult life, including adult health care, work, and independence.
Challenges:
- Lack of information about current services and experiences of adults with ASD.
- Lack of appropriate education and training of families, professionals, and community.
- Ineffective transition planning and coordination of services.
- Few services tailored to adolescents and adults.
- Few services and no entitlements available for adults with ASD.
Recommendations:
- Collect data about the life experiences and needs of adults with ASD.
- Start transition planning services early.
- Develop and support skill-building opportunities that promote self-determination in youth with ASD.
- Provide an array of services and supports in the community for individuals with varying degrees of ability.
- Incorporate aging issues into transition planning such as estate planning and long term care.
- Formalize Federal partnerships to ensure collaboration across service sectors providing transition planning.
- Establish an interagency Federal task force that identifies the needs of adults with ASD and determine how best to meet them.
VI. Appropriate Financing of Care
Appropriate financing of services and affordability of treatment are considered the most important enabling factors associated with timely access to care. For individuals with autism and their families, however, the lack of appropriate financing is most frequently identified as a barrier that impedes access to services. Inadequate reimbursement contributes to the lack of adequate numbers of qualified health professionals in the field and ultimately lack of available services. Given the complexity and breadth of the financing mechanisms for health, education, and social services, the EWG focused on privately/publicly financed health insurance, and publicly financed education and social services programs for ASD and the importance of the interactions and coordination of financing mechanisms essential to care for people with ASD.
Private health insurance plans are seriously inadequate in financing ASD services. Employer-based private health insurance in general excludes developmental disabilities, including ASD, from their benefit coverage. ASD is also excluded from coverage because it is considered by the insurance plans as a non-medical condition to be handled by the educational system, or a mental health condition with limited coverage. Given that ASD still lacks widely-recognized and uniform standards for diagnosis and treatment and is considered a chronic condition requiring continuous services throughout an individual's life with associated high costs, insurance companies and managed care plans are inclined to limit coverage to control costs.
During the last decade, new treatment approaches have been developed for ASD and a number of states have mandated coverage in employer-based health insurance plans. Unfortunately the effectiveness of the service coverage content of these plans is still not known. A major shortcoming is that many health plans are offered by self-insured employers, and these are exempt from state mandates under the Employee Retirement Income Security Act (ERISA). In those self-insured employer plans that do provide coverage for their employees and their dependents, time limits of coverage are often present.
Medicaid is the most significant publicly financed health insurance program for individuals with ASD and their families, however many adults and children are not covered by Medicaid because they have higher income than the Medicaid eligibility criteria. Some Medicaid waiver programs have been initiated that provide eligibility for children up to age 21, regardless of the parents' income level. Currently, most of the ASD-related specialized services are covered under waivers submitted by States and granted by the Center for Medicare and Medicaid Services. These waivers request that providers of services for ASD include schools, early intervention programs, and specialized ASD services programs, and can bill Medicaid for their specialized services. Requesting reimbursement for case managers with ASD-specialized skills is also part of these waivers. However, these waiver programs are not consistent from state to state and in many cases, parents report long waiting times for these covered services. Long delays in accessing needed services are unacceptable from a public health perspective. One of the most important principles of public health is that while research focuses on discovering the cure for an illness, those who are already suffering from the illness should have easy access to existing treatment in a timely manner.
Publicly financed education and social services for ASD are primarily financed through state and local revenues that support independent and often fragmented programs and services that vary greatly from place to place. Where such funding is available, it is very limited and requires that families and providers submit large volumes of burdensome paperwork to negotiate the fragmented system. Most funding for developing coordinated systems of care is available on an experimental or demonstration basis.
Goal: To expand and standardize public and private financing of ASD-related services so that individuals with ASD and their families have access to early and continuous screening, comprehensive diagnosis, and needed health/mental health, education, and social services.
Challenges:
- Inappropriate restrictions on eligibility criteria for people with ASD.
- Inadequate benefits in public and private insurance programs.
- Inadequate provider reimbursement for appropriate ASD-related services.
- Lack of flexibility in publicly financed service programs.
- Inconsistency across states and localities and the lifespan in mechanisms to pay for services.
- Lack of assistance to families in providing for the financial needs of individuals with ASD.
Recommendations:
- Demonstrate the cost-effectiveness of early intervention.
- Expand health insurance benefits for ASD, taking into account the need for a broad array of services.
- Develop model financing, public/private insurance packages and Medicaid waivers.
- Conduct a national study of cost and insurance to determine policies and practices that affect financing, eligibility, and service delivery.
- Adapt innovative approaches, such as use of tax-exempt medical savings accounts and financial planning assistance, strategies that blend funding from multiple sources to create a coordinated approach to financing.


